This week Jill and I have been to Brussels for the third International COVID (Crisis) Summit. This meant hotel buffet breakfasts, heavy lunches, which were followed by even more “heavy” Belgian dinners. Deserts, sweets and alcoholic drinks available at every meal. What’s not to like? Well, basically, if you are like me, that is a person of a “certain age,” who is slightly overweight and who struggles with elevated glycemic levels, basically everything.
Over the past six months, Jill and I have taken our health more seriously than ever before. We have taken to eating two meals a day, as close together as possible to promote autophagy. We keep sugar out of the house, eat very little bread and generally work hard to eat clean. For the most part, we buy organic foods.
At age 63, I have a tendency to binge on food, and as my glycemic levels have crept up, so have my cravings for sugars and simple carbs. So much for the Italian pasta dishes that I love! The only way I can control simple carbs effectively is to avoid them at all costs. Unfortunately, my sugar/simple carb cravings take the form of “drug seeking behavior”, and I have to not indulge or frankly, I binge. When we are on the farm, I am able to get outside. Doing chores and getting exercise happens on the farm without a lot of thought. When traveling, sometimes it seems like the most exercise we get is getting to our next gate at the airport.
With the help of a great physician, Dr. Brooke Miller – who works to keep me and all his patients on the straight and narrow path of healthy eating, I have lost weight, regained stamina and have more exercise tolerance. But traveling is both stressful and full of unhealthy food choices. It is also a necessary evil for accomplishing this educational mission that I have set myself to - so it is a constant struggle.
This morning over an unhealthy breakfast in Brussels, Dr. Brooke Miller (who was also attending the summit) and I were discussing what truly is a health crisis in America. That is the lack of metabolic health in America.
He posed the question, “what if instead of pushing vaccines, the government instead had promoted the importance of “metabolic health?” in reducing the severity of COVID-19 disease. What if our elders had been told to exercise more, eat healthy, control blood sugars, take vitamin D (+ other needed supplements) and lose weight? That it was imperative to increase metabolic health for the general population, and particularly for those of us who are older and tending towards too many pounds.
One of the most important points Dr. Miller made during the discussion is the strong link between vitamin D deficiency and obesity. People who are obese tend to be vitamin D deficient. The truth is that most Americans are both overweight and vitamin D deficient, and this is not a coincidence.
Just think what that means in terms of infectious respiratory disease, including COVID-19. Was the severe disease seen in obese patients during the COVIDcrisis largely driven by metabolic syndrome, high glycemic levels or vitamin D deficiency or some synergy of all three? Regardless of the answer, suffering from metabolic syndrome can have significant health consequences for even something as simple as catching a case of flu, not to mention COVID.
So, understanding metabolic health is important. In the United States (2018 data), the percent of adults aged 20 and over who are overweight, including obesity was 73.6%. Over 42% of adult Americans are obese.
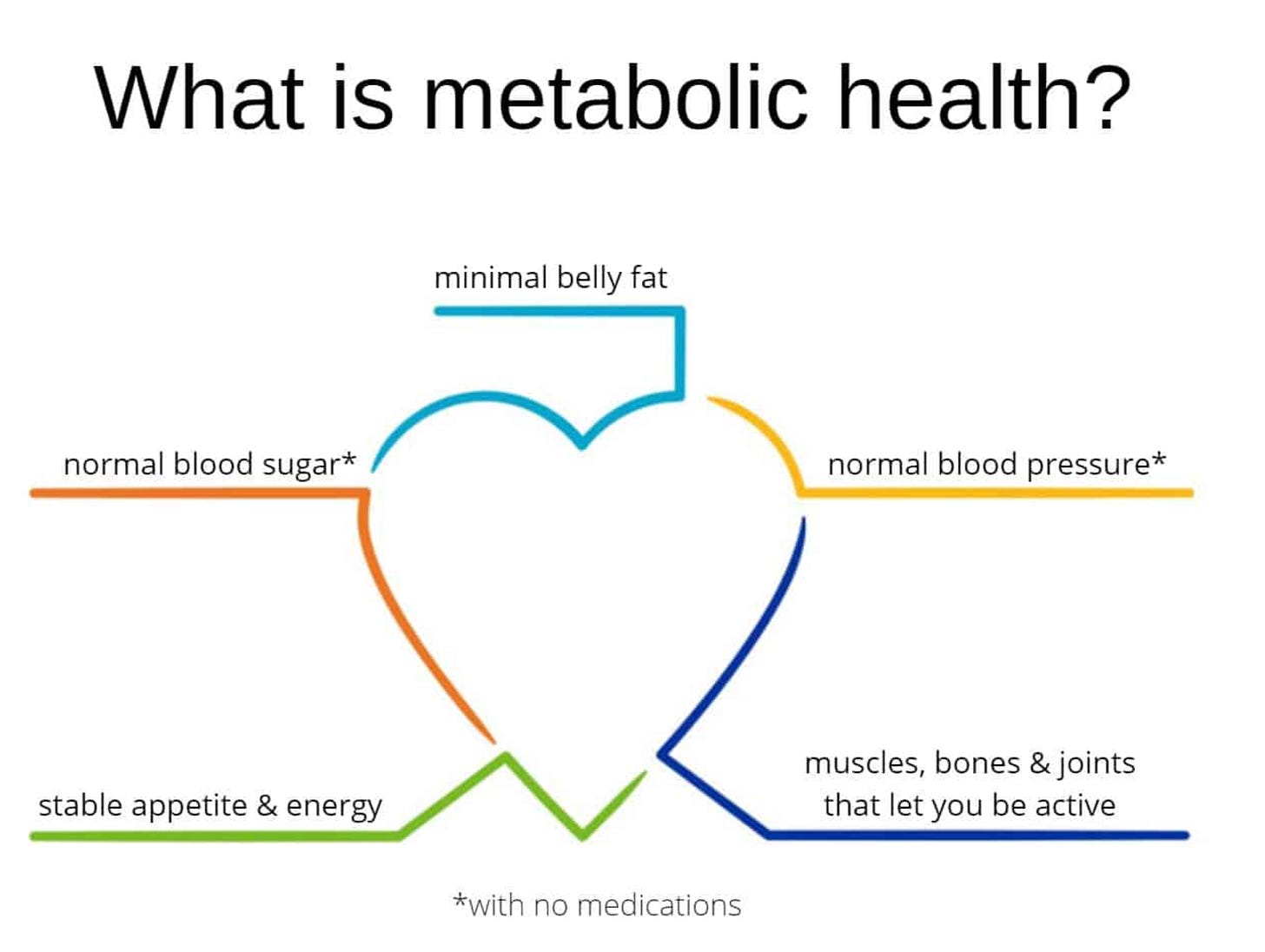
What is metabolic health? The definitions on the net run from the most general description, such as: “Metabolic health is a term to describe how well we generate and process energy in the body”, to much more detailed and specific definitions.
Here is a diagram that I think is very useful way to think about it:
Of course, if one understands what metabolic health is, then the next questions might be, “so what is an unhealthy metabolism?” or “What is metabolic syndrome?”
What is metabolic syndrome?
Metabolic syndrome refers to the presence of a cluster of risk factors specific for cardiovascular disease. Metabolic syndrome greatly raises the risk of developing diabetes, heart disease, stroke, or all three.
According to the National Heart, Lung and Blood Institute (NHLBI), the cluster of metabolic factors involved includes:
Abdominal obesity. This means having a waist circumference of more than 35 inches for women and more than 40 inches for men. An increased waist circumference is the form of obesity most strongly tied to metabolic syndrome.
High blood pressure of 130/80 mm Hg (millimeters of mercury) or higher. Normal blood pressure is defined as less than 120 mm Hg for systolic pressure (the top number), and less than 80 mm Hg for diastolic pressure (the bottom number). High blood pressure is strongly tied to obesity. It is often found in people with insulin resistance.
Impaired fasting blood glucose. This means a level equal to or greater than 100 mg/dL
High triglyceride levels of more than 150 mg/dL. Triglycerides are a type of fat in the blood.
Low HDL (good) cholesterol. Less than 40 mg/dL for men and less than 50 mg/dL for women is considered low.
The NHLBI and AHA recommend a diagnosis of metabolic syndrome when a person has 3 or more of these factors.
Most people who have metabolic syndrome have insulin resistance. The body makes insulin to move glucose (sugar) into cells for use as energy. Obesity, commonly found in people with metabolic syndrome, makes it more difficult for cells in the body to respond to insulin. If the body can’t make enough insulin to override the resistance, the blood sugar level increases, causing type 2 diabetes. Metabolic syndrome may be a start of the development of type 2 diabetes.
Because the population of the U.S. is aging, and because metabolic syndrome is more likely the older you are, the American Heart Association (AHA) has estimated that metabolic syndrome soon will become the main risk factor for cardiovascular disease, ahead of cigarette smoking. Experts also think that increasing rates of obesity are related to the increasing rates of metabolic syndrome.
What causes metabolic syndrome?
Experts don't fully understand what causes metabolic syndrome. Several factors are interconnected. Obesity plus a sedentary lifestyle contributes to risk factors for metabolic syndrome. These include high cholesterol, insulin resistance, and high blood pressure. These risk factors may lead to cardiovascular disease and type 2 diabetes.
Because metabolic syndrome and insulin resistance are closely tied, many healthcare providers believe that insulin resistance may be a cause of metabolic syndrome. But they have not found a direct link between the two conditions. Others believe that hormone changes caused by chronic stress lead to abdominal obesity, insulin resistance, and higher blood lipids (triglycerides and cholesterol).
Other factors that may contribute to metabolic syndrome include genetic changes in a person's ability to break down fats (lipids) in the blood, older age, and problems in how body fat is distributed.
Who is at risk for metabolic syndrome?
Knowing your risk factors for any disease can help guide you to take the appropriate actions. This includes changing behaviors and being monitored by your healthcare provider for the disease.
Risk factors most closely tied to metabolic syndrome include:
Age. You are more likely to have metabolic syndrome the older you are.
Ethnicity. African Americans and Mexican Americans are more likely to get metabolic syndrome. African-American women are about 60% more likely than African-American men to have the syndrome.
Body mass index (BMI) greater than 25. The BMI is a measure of body fat compared with height and weight.
Personal or family history of diabetes. Women who have had diabetes during pregnancy (gestational diabetes) or people who have a family member with type 2 diabetes are at greater risk for metabolic syndrome.
Smoking
History of heavy drinking
Stress
Being past menopause
High-fat diet
Sedentary lifestyle
The article above mentions insulin resistance as being one of the primary indicators of metabolic syndrome.
There are two primary ways to reverse insulin resistance without the use of drugs. The first is eating healthier foods and the second is exercise, which has been shown to make the body more sensitive to insulin.
There is also a link between metabolic syndrome and inflammation.
The proinflammatory state that accompanies the metabolic syndrome associates with both insulin resistance and endothelial dysfunction, providing a connection between inflammation and metabolic processes which is highly deleterious for vascular functions (RWM: ergo - cardiac disease).
An inflammatory state and metabolic syndrome is associated with not only cardiac disease but also auto-immunity, including rheumatoid arthritis.
Patients with rheumatoid arthritis suffer increased heart disease over and above traditional risk factors. They have an increased occurrence of metabolic syndrome that enhance the risk further. Metabolic syndrome occurs early in the course of rheumatoid arthritis, creating clinical opportunities for prevention and control. Patients with both conditions also have more severe disease, pain, poorer functional status, less remission rates, and suboptimal response to treatment. Treatment of metabolic syndrome should be aggressive, using a proactive approach. Lifestyle measures are a corner stone, and this should be coupled with optimal control of rheumatoid arthritis, blood pressure, and lipid levels.
Clearly, I have metabolic syndrome which has developed during the last three years, if not before. Maybe this is part of the reason why my initial infection with Wuhan-1 SARS-CoV-2 in late February 2020 hit me so hard. I can partially blame COVID and the vaccine for many of my current symptoms, but the truth is that I let my BMI creep up just enough, I have a genetic profile that is susceptible, the pseudo mRNA vaccine caused hypertension/Tachycardia/POTS, and I let myself use food as a reward when stressed. All together, was the perfect storm.
Thirty percent of adult Americans have metabolic syndrome, and this is even more prevalent in my age cohort. Over forty percent over the age of 40 have metabolic syndrome.
My hope in sharing this story of my struggles in controlling my metabolic health, I can inspire others to do likewise. Here is the thing, I am not perfect. I know this, but I have been working hard to overcome my health issues. I am 63 years old, I will never be a young man again. However, I am improving my health, I am making progress - really one day at a time. And it does take time.
I think most people know that finding a solution to improving one’s metabolic health that you can “live with” is vitally important to living a long, high quality life. Yet there is no simple solution, no one answer on how to do it. We each have to come to that answer on our own.
It is something I have to grapple with everyday, but so should the 74% of Americans who are overweight. This is not easy. Food is addictive. Sugar is essentially a drug of abuse.
This is what has worked for me:
Putting myself on a schedule of intermittent fasting (two meals a day).
Cooking only what I should eat to control eating too much (portion control).
Eat a small portion and then wait, let it settle, before eating any more.
Eating enough protein.
Not eating many simple carbs and sugars (almost a keto diet).
Making sure I routinely get outside, with some sort of exercise, even if it is just walking
Getting myself away from the computer and cell phone.
I wish I could add “avoid too much travel and hotel food” to the list, but there it is. Maybe someday.
Changing habits is hard, I know. But I am slowly having success, and you can too.
Health is important. I hope and trust that we are on the same page about this.


Dr. Malone - I remember, in my much younger days looking at the corruption in our world and feeling so small and alone. One of the great ironies of life is that through this hideous travesty called COVID, we have come to find you and the stellar humans like you, Pierre Kory, Paul Marik, Aseem Malhotra, Tess Laurie, Bonnie Ann Cox, Jessica Rose, A Midwestern Doctor, Bobby Kennedy. I am so inspired by all of you.
A wise man once said, “I truly believe we are at a pivotal time, where the work that each of us puts in can make an immense impact on the future course of this world.”
I, for one, am inspired to act upon that advice.
Thank you. I am eternally both grateful and indebted to you folks - for saving me from despair. ☺️
This is right on target.
My only additional comment is we fast 36 hours a week.
Dinner on Saturday is our last food of the week.
No food - only water tea coffee and an electrolyte drink on Sunday.
Breakfast ( break fast) Monday morning
I am very ketotic by Monday morning. Ketosis suppresses hunger by the way.
Interestingly, I am not hungry Monday morning, feel physically great and mentally more clear than any other time of the week
Doing this, and eating only 2 meals a day is how I lost 40 lbs and have kept most of it off